Team Care Medicine Podcast Interview with Dr. Dike Drummond
By: Steve Moberg
Chief Operating Officer at Team Care Medicine, LLC
In the on-going battle to combat physician burnout, many hospital administrators and / or physician group leaders desiring to help, face the dilemma of adding yet more costs to an operation likely already struggling to turn a profit. In other cases, when administration is not providing the help, many exasperated doctors are paying for a scribe out of their own pocket.
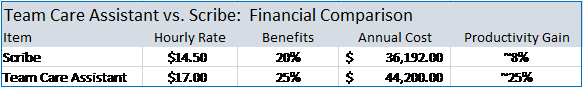
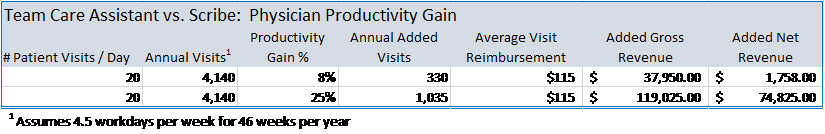
The burnout issue is real and hiring a scribe to help with the heavy EHR documentation burden is becoming a common approach to solving it. A few years ago, the College of Medical Scribe Specialists predicted 100,000 scribes would be employed by 2020. With the Covid Pandemic, it is hard to tell exactly where the number stands today but the bottom line is it is a fast-growing solution. At about $15 per hour (a rough national average ) the annual expense with benefits can reach $25,000 to $35,000. So desperate is the situation, they add this expense with no guarantees of financial returns sufficient to pay for it. Yes, a scribe will bring some relief from EHR documentation, but the resulting productivity gains are mixed. Some doctors see a 6%-8% (the high end of the range) productivity lift, however, a 2019 $480,000 scribe model pilot at St. Charles Medical Group in Bend, Oregon was scrapped because the “modest” productivity gains (only ½ a patient visit added per day) were insufficient to pay for the scribes. For about the same cost, administrators could upgrade to a more powerful solution that has been proven to boost physician productivity by 20%-40% or higher. That kind of productivity gain will easily pay for an additional MA being added to the team in lieu of a scribe. In this article, we will compare a Team Care Assistant (usually an MA trained in the use of the Team Care Medicine Model) to the use of a typical medical scribe. We will evaluate what they do and the benefits each provides.
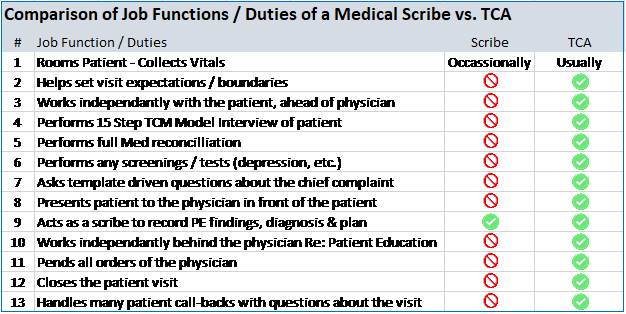
A medical scribe is quite simply a person that interfaces with the Electronic Health Record (EHR) during a patient visit freeing the doctor to focus on the patient. In most situations they require no specific certification or formal training to perform these duties. Candidates that possess soft skills like good listening, good communications, computer (typing) skills as well as some knowledge of human anatomy and medical terminology have an advantage. A high school diploma is a requirement and some background or courses in medicine is a benefit. Typically, a pre-med student is a good candidate however eventually they will move on so turnover may be an issue. A certification program is also available from the American Healthcare Documentation Professionals Group. In most cases, the medical scribe is not in the exam room independent of the physician other than to perhaps room the patient and collect a few vital measurements (temperature, blood pressure, etc.). Lastly, they are not nurses, or even MAs, so there are functions they cannot do which limits their versatility in the practice.
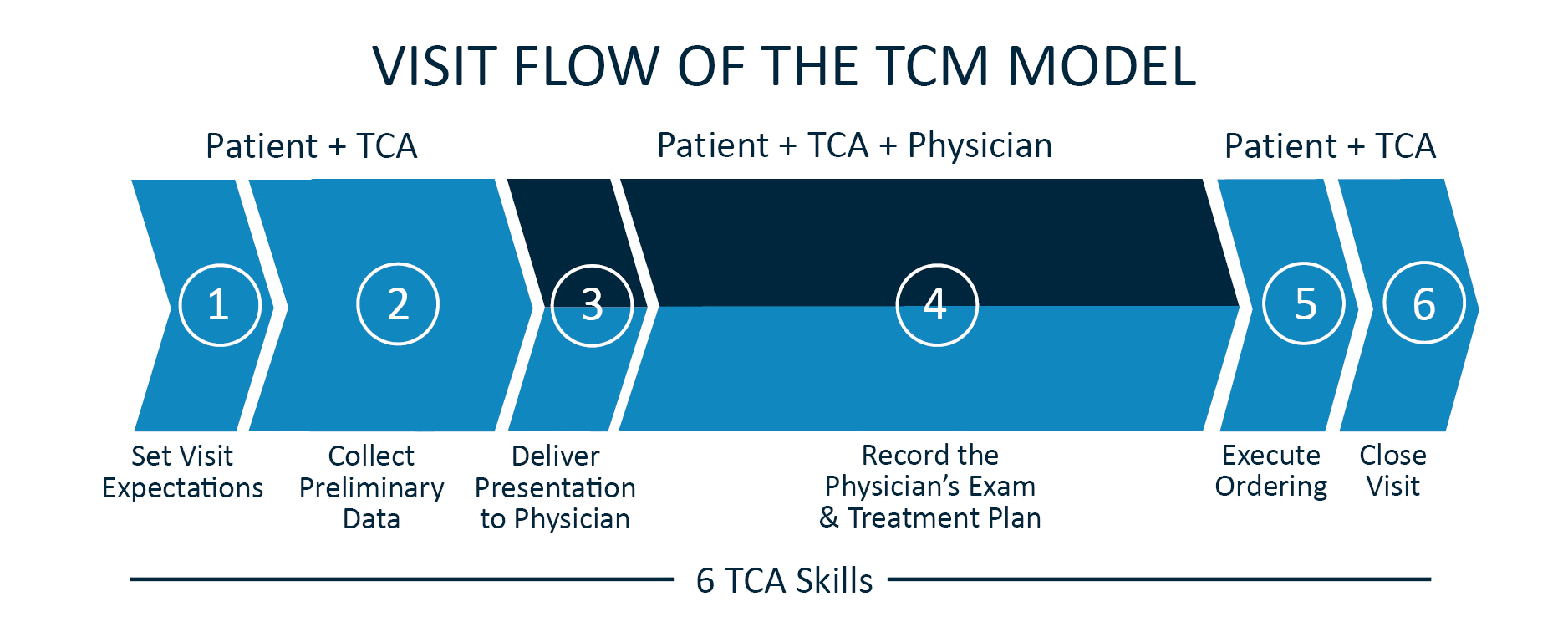
A Team Care Assistant (TCA) is usually a Medical Assistant (MA) or less often a Nurse (LPN or RN) trained by Team Care Medicine to execute a patient visit using the Team Care Medicine Model. The TCA is with the patient throughout the patient visit. They greet the patient and begin their 15-step process (fewer steps for an urgent visit) of interviewing the patient to capture all the patient’s medical information including the use of template driven questions about the chief complaint. Once all the patient’s medical information has been collected and updated in the EHR, the TCA notifies the physician, and the physician enters the exam room. The 5-15 minutes of data collection is then presented in a 2-3 minute crisp, data packed presentation to the physician in front of the patient. After presentation, the TCA then performs the role of a scribe, documenting any additional questions of the provider and answers of the patient. They also document any physical exam findings as well as the diagnosis and treatment plan of the physician in the EHR. Once the doctor has completed explaining the treatment plan to the patient, the doctor is free to exit the exam room and leave the TCA to again go over the treatment plan, perform any patient education and close the visit. See the following diagram of the Team Care Medicine visit flow.
There are meaningful differences between a scribe and a TCA in the work they perform, the satisfaction they bring to patients and in the superior financial benefit they produce making the TCA a much more valuable addition to the team than a scribe.
The scribe is generally in the exam room only when the physician is in the exam room. The TCA, as outlined above works independent of the physician during portions of the visit. This is where the significant time savings occurs. A scribe does not collect the patient’s information beyond vitals, nor do they present this data to the physician. A Scribe cannot perform medical procedures or screenings (such as for depression) because they have no medical training. A TCA on the other hand can perform these tasks. A Scribe does not do patient education or review the plan of the provider or close the visit allowing the doctor to slip out sooner, however, a TCA does all these things. A scribe does not take calls from patients with questions about their visit while the TCA fields many of the after-visit patient calls, protecting the physician from work that could easily be done by someone else. A TCA also helps set patient expectations such as helping to keep an urgent visit to just one issue or to let the patient with a list of 10 items know that the doctor will be made aware of them all but may only be able to evaluate 2 today and that an additional appointment(s) may be needed to cover the rest. A scribe does not engage in anything like this. Finally, the TCA working with the physician as a team just gets more done and it is done more efficiently, just like an OR Nurse helps the surgeon inside the operating room. All these differences add up to be significant benefits to the doctors and to the patients throughout the year. The benefits of a scribe are limited because the scope of work they perform is narrower than a TCA’s. See Table-1 For a summary comparison of the differences between a TCA and a Scribe.
With all the tasks on the plate of a primary care doctor working alone during a patient visit, it is easy for a patient to walk out the door at the end of the visit wondering if the doctor was really listening to them. When they hear the TCA crisply deliver their story to the physician and realize all the data points associated with their care, they know they have been heard. When the doctor explains the treatment plan and then the TCA repeats it and reviews the entire visit, they leave with a better understanding of the plan and what the doctor is asking them to do. Additionally, a 2019 ASHP Survey showed patients are less likely to ask questions about the care plan when they feel the providers are stressed and need to move on. They would more likely ask their questions to the TCA as they feel the TCA is more on their level. When they feel like they truly have a care team looking after them, it is very patient satisfying, and they view it all as better care.
The TCA is there to significantly increase the efficiency of the physician by doing ALL non-physician work. It takes 2.5 TCAs for a physician to use the Team Care Medicine Model on 100% of the day’s patient visits. Most offices already have 1 to 1.5 clinical assistants per provider. Therefore, usually just 1 additional MA needs to be hired to round out the team. While the doctor and TCA #1 are in Exam Room #1 with Patient #1, TCA #2 is in Exam Room #2 with Patient #2 collecting all their relevant medical information and setting the table for the doctor to enter. When the doctor goes into Exam Room #2 with TCA #2 and Patient #2, TCA #1 wraps up the visit with Patient #1 and then begins the visit for Patient #3. See Diagram-2 depicting the provider hourly workflow.
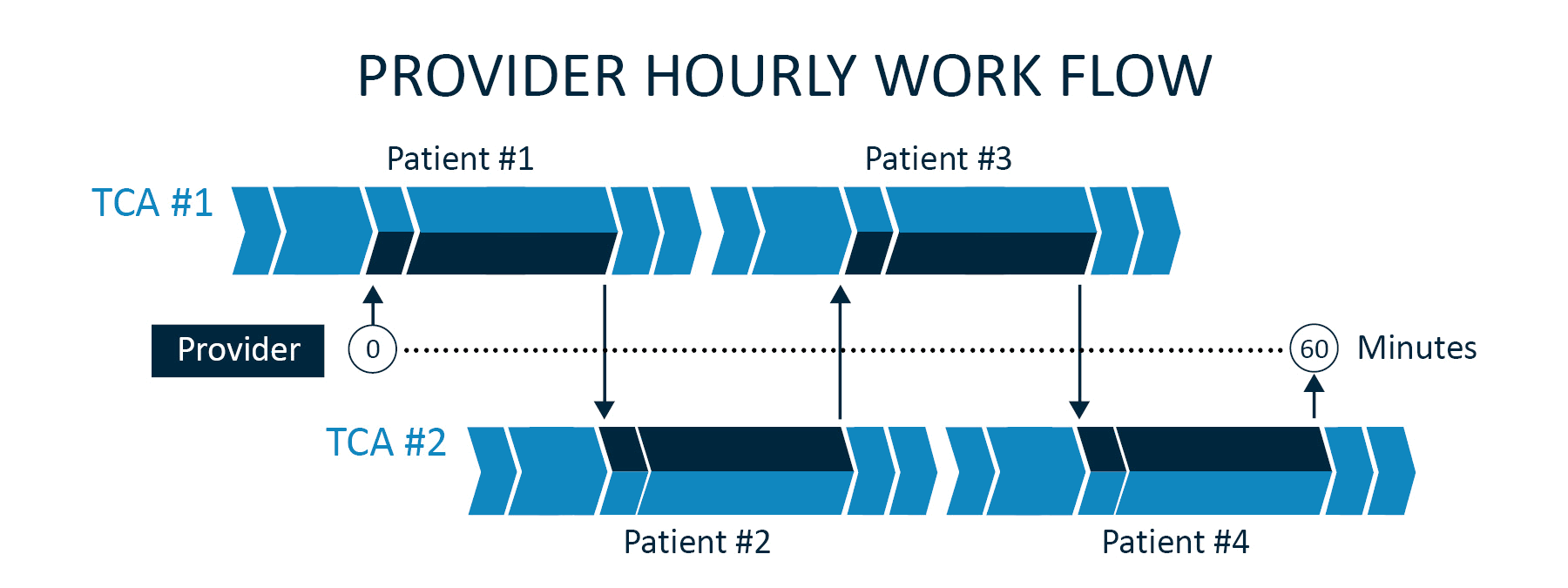
This “dance” is repeated all day with the doctor going from exam room to exam room doing just the work that only they can do. The TCM Model flow also creates natural gaps throughout the day providing doctors a few minutes to knock out an item or two on their task list resulting in less work at the end of the day before heading home. The ability of a TCA to work independent of the doctor produces the big productivity boost over the scribe option. Otherwise, the patient visits are accomplished serially with the doctor and the Scribe doing each together. The TCA typically delivers a 20-40% productivity gain in visit volumes with similar gains in the amount of work they accomplish as a team during the visit (Work RVUs). They help the doctor see more patients and get more done during the patient visit. With similar costs (See Table-2) you get much more bang for your buck with a TCA as opposed to a Scribe (See Table-3).
A Team Care Medicine TCA paired with a motivated doctor looking for a solution to burnout while desiring to maintain the highest level of care for their patients is an overall more powerful and efficient solution than a medical scribe model. Administrators hesitating to add more expense to their primary care offices should have great confidence that they can now add the needed help and that doctors can generate enough additional revenue to more than cover the added expense.
Listen to three medical assistants (MAs) describe the transformational experience of serving in the Team Care Medicine (TCM) Model. They’re more fulfilled in their work, their providers are delivering better care, and patients are delighted.
Dr. Juli-Anne Wade describes the many benefits she has enjoyed since implementing the TCM Model at her practice nearly four years ago. Team Care Medicine has helped hundreds of doctors around the country implement the TCM Model. Dr. Wade, a pediatrician at the University of Virginia, University Physicians Group is one of them. She completed her medical training and residency at UVA after earning a bachelor’s degree in Biology. She opened her Fishersville practice in 2013 and she and her husband have two children. Her discussion of the TCM Model follows.
We are continuing our series of interviews with providers across the country as more and more practices adopt the TCM Model. In this edition, we hear from Dr. Gina Engel of
UVA Physicians Group (Virginia). She completed her education and residency at Virginia Commonwealth University’s Medical College of Virginia. Dr. Engel adopted the TCM Model in 2018. What follows are her reflections.
By: Steve Moberg
Executive VP and COO at Team Care Medicine, LLC
This article is the third in a three-part series on the costs of physician burnout. The first installment provided the financial perspective while the second examined the physician’s personal perspective. This third round focuses on the cost to patients resulting from physician burnout.
Most patients are unaware of the physician burnout epidemic and its causes. Nevertheless, it increasingly affects the care they receive. Patients may wonder why it has become more difficult to make an appointment with their primary care doctor or why their doctor seems distracted during the exam. Patients are surprised when they must ask their doctor, “Isn’t it about time for my next colonoscopy?” instead of the doctor identifying the care gap. They are frustrated when they cannot get in to see the doctor for an urgent issue, forcing them to visit the emergency room at far greater expense. Patients may not know to label these as consequences of physician burnout but they are aware of these changes and how it impacts their lives and care.
Dr. Peter Anderson, founder of Team Care Medicine and a 30-year primary care doctor, identified accessibility, attentiveness, and accuracy as the three pillars necessary to achieve patient satisfaction and quality of care. Physician burnout is now quickly eroding each of these three critical foundations upon which so many doctors have built their practices.
Access to care is the single most important determinant in patient quality of care — after all, there’s no care if the patient can’t see the doctor! An array of forces is driving a large and growing shortage of primary care doctors, and none is more insidious and preventable than physician burnout.
Demographic trends are driving increased demand for health care, with the US population growing and aging rapidly. While the total US population is projected to increase 10.3% by 2032, the population aged 65 and over is projected to grow by 48.0%, driving demand for care much more rapidly than the overall population growth would imply.
Meanwhile, physician burnout is eroding the supply of primary care on several fronts. First, burnout is causing practicing physicians to reduce their care hours. Physicians trade patient time for admin time to catch up on charts and other administrative tasks. Second, burnout is causing practicing physicians to retire earlier. With 42% of primary care physicians over age 55, this is an acute and growing risk. Third, as medical students perceive the high dissatisfaction of primary care physicians, fewer are choosing this career path.
Increasing demand and eroding supply conspire to paint a bleak picture for patient access to care. A primary care physician shortage of 38,000 physicians is projected by 2032. The AAFP found that an increase of one primary care physician per 10,000 population was associated with 15.1 fewer deaths per 100,000 as well as 39.7 fewer ACSC hospitalizations per 100,000 and 712.3 fewer ED visits per 100,000. Real solutions are desperately needed to unlock patient access to care and thereby reduce ED visits, hospitalizations, and deaths.
Patients reasonably expect their physician to be mentally present and focused during the exam. However, a common symptom of burnout is emotional disengagement. When patients feel their doctor is already under personal strain or overwhelmed, they tend to pull back and not share all their issues or ask all their questions. They do not want to add to the doctor’s level of stress, so they don’t. With less information available, the ability of the provider to offer quality patient care is obviously diminished.
One major contributor to burnout is the burden of administrative tasks and EHR Patient Chart documentation. To minimize the amount of chart documentation to be done later, many physicians feel compelled to enter data in the EHR even as they interact with the patient. Carrying on simultaneous “conversations” with the patient and the computer is exhausting for the physician and leaves all parties dissatisfied. So, not only is the burned-out physician emotionally unavailable to the patient during the visit, he/she exacerbates his/her emotional burnout by trying to maintain two conversations at once, continuing the vicious cycle. Meanwhile, the patient doesn’t feel heard and doesn’t share as much information, with dire consequences for health, not to mention patient satisfaction.
As detailed in an earlier TCM missive on the financial cost of burnout, quality of care is jeopardized when a physician begins to experience burnout. Patients need a physician practicing at the top of his/her capabilities in order to keep up with the increasing complexity of primary care. Otherwise, missed pre-emptive screenings for cancer, errors in judgement when developing care plans, or charting errors can emerge. The 2019 Medscape Survey revealed 26% of depressed doctors say they are less careful when completing the visit documentation and 14% said they are making errors they wouldn’t ordinarily make. Survey results in a recent Mayo Clinic Proceedings article suggest a burned-out doctor is 120% more likely to make a medical error than a doctor that is not.
Burned-out physicians do not need to learn new breathing techniques or other mechanisms to cope with stress. They need real solutions.
In the InCrowd 2019 Survey, doctors were asked what they needed from their administration to help combat burnout. The number one answer by 66% of the doctors was to add staff. They understand that many of the tasks they perform each day can be performed by support staff. However, this is only part of the solution. Physicians need to reconceptualize their own role while surrounding themselves with a well-coached and properly equipped exam room team.
The TCM Model eliminates burnout and restores the joy of medicine. In this system, the role of the physician is upgraded from overloaded work horse to team captain. The clinical support staff (usually MAs) are equipped to operate up to the limit of their license. They perform 7 new skills, including the bulk of the EHR documentation. This relieves the physician of all unnecessary administrative burdens before, during, and after the visit. With a larger team of higher functioning clinical support staff, the physician is able to concentrate on the patient (not the EHR), and focus on diagnosis and care decisions — the reasons they went to med school.
Access improves as daily visit volumes and work RVUs increase 20-40%. Patients can once again see their regular primary care doctor rather than a rotating cast of urgent care centers, emergency departments, etc.
Attentiveness improves as the provider is freed from EHR data entry. As one recent convert observed: “I never realized how stressful it was to have to carry on two conversations at once until I no longer had to do it.”
Accuracy improves as the provider’s emotional wellbeing is restored, boosting patient health and satisfaction.
Dr. Chaoui, president of the Massachusetts Medical Society, noted that “We need to take better care of our doctors and all caregivers so that they can continue to take the best care of us.” The TCM Model takes good care of the providers and, by extension, their patients.
Emotionally healthy physicians make a life-saving impact on their patients every day. Here’s just one example: When Dr. Peter Anderson developed the TCM Model, he equipped his Team Care Assistants (TCAs) to collect background data from each patient before the exam formally began, affording the TCA an opportunity to ask a number of profile questions that Dr. Anderson often ran out of time to ask himself. One day, Howard, a 54-year-old male, had an appointment to evaluate a lesion on his scalp. While the TCA was going through her routine data gathering, she asked Howard the profile questions for which he qualified: “Do you ever have any pain in your chest or shortness of breath when mowing the grass, carrying in the groceries, or going up stairs? And if you rest a minute, does the pain/shortness of breath subside?” Howard pondered for a moment then responded: “You know, I have had some pain in my chest the last couple of times I mowed the grass but it went away when I was done so I kind of just forgot about it.…so yeah, I guess I did!” The TCA made a note of it in the chart and during her presentation of Howard to Dr. Anderson, she passed the information on to him. Dr. Anderson asked a few more questions of Howard and told him he needed a stress test. Howard received a triple bypass three days later. Without the TCM Model, Dr. Anderson often did not have time for these profile questions orthogonal to the purpose of the visit. With the TCM Model, Howard’s life was saved through high quality care by an emotionally healthy provider supported by a high functioning exam room team.
For more information, go to www.wordpress-603318-1953014.cloudwaysapps.com.
This article is the second in a three-part series on physician burnout. The first installment focused on the financial costs of physician burnout. This second article focuses on the human or personal side of physician burnout.
In early 2019, Dr. Miller was preparing to quit his hospital-owned practice near Cincinnati to launch his own concierge practice (we’ve changed his name to protect his privacy). Dr. Miller loved his patients, he didn’t want to do this, but he was trapped in a patient care model that was failing him. He found it impossible to provide the care he wanted to his patients while maintaining a life outside of medicine. The updating of patient’s charts in the EHR was totally dominating his evenings and weekends. He was single and hadn’t been on a date in months.
As his frustration and dissatisfaction peaked, he decided to make the difficult change to a concierge model. The disruption for him, his patients, and his soon-to-be-former employer would be very costly, but he just couldn’t take it anymore.
Sadly, stories like Dr. Miller’s are repeated all across the country. Long-term unresolved job stress has led doctors to feel exhausted, overwhelmed, cynical, and detached. A recent Mayo Clinic Proceedings article concluded that doctors are 50% more likely to battle emotional exhaustion than the average American worker. Primary care physicians are particularly susceptible – they’re 40% more likely to experience burnout than specialists.
As a result, many physicians are looking for an exit. They are seeking administrative jobs to reduce patient time or have accepted a half-day or even a full day of “admin catchup time” to avoid the negative impact on their families, to the detriment of their paycheck. Other doctors are simply retiring earlier than planned to escape the grind. Still others are transitioning to different practice models altogether. Many fantasize about quitting medicine and starting a new career. Collectively, these escapes reduce patient access without solving the underlying problems that precipitate burnout.
For physicians that are unable to escape, many feel the walls closing in month after month. They become disenchanted with their profession, even hating medicine. They detach from their families and friends. Medscape’s National Physician Burnout & Suicide Report of 2019 found nearly 4% of US doctors (35,000!) are clinically depressed. Tragically, some have even turned to suicide to end the misery. One doctor commits suicide in the U.S. every day – the highest suicide rate of any profession. And the number of doctor suicides – 28 to 40 per 100,000 – is more than twice that of the general population. It’s no surprise that solving physician burnout ranks in the top 5 on most hospital CEO’s list of priorities.
Burnout starts with long hours: the average physician works 52.6 hours per week, or 30% more than the average US worker. It’s even worse for the 40% of doctors that work more than 60 hours each week. However, having persevered through medical school, long hours are not the sole cause of burnout. The nature of the work is just as much of an issue. With more and more time dedicated to data entry in EHR charts, many doctors have gradually lost their personal connection with their patients – they’ve lost the “Joy of Practicing Medicine”.
The tremendous pressure to close charts causes many physicians to feel they are simply a cog in the healthcare machine with no higher purpose than capturing revenue. They long for the day when they felt like a valuable knowledge resource, like a practitioner of medicine with an essential vocation. What they thought they were signing up for is NOT what they are experiencing.
Physicians’ families have a front row seat to the destructive power of burnout. Spouses, kids, parents, and friends all see the internal battle between a desire to deliver quality care for their patients and their need for a personal life.
After a full day of patient visits (often feeling pressured and running behind by the end of the day), many physicians come home, feed the kids, help with homework, rush the kids to bed, and then jump back on the computer for 2-3 hours of additional chart work. Spouses are forced to pick up the slack, often causing more stress and friction at home.
Burnout manifests itself in increased isolation, greater irritability, more time away from home, less communication, less time together, a drop in physical intimacy, and emotional separation. Frayed relationships at home only add more pressure on the physician. A real-world solution is desperately needed.
Given the breadth and depth of the problem, a variety of solutions have been tested to combat physician burnout, often having little or no effect. Sadly, many so-called solutions fail to tackle the underlying issues and instead apply “Band-aids” like meditation, breathing exercises, and relaxation techniques.
A recent InCrowd Survey asked physicians what they wanted their hospital administrators to do to help them combat physician burnout. Their #1 response (at nearly 66%) was to add more staff to help ease the administrative/documentation burden. Any serious attempt at solving the burnout problem needs to take this information seriously.
One common approach is hiring a scribe for each physician to interface with the EHR, a bit like a “human app” added to the computer. While this is a step in the right direction, the scribe model comes with a significant limitation: because the doctor is still in the exam room throughout the entirety of every patient visit, scribes don’t provide a boost in productivity sufficient to pay for their additional cost. As a result, hospital executives choosing this solution simply add more cost to primary care offices which are usually already operating deeply in the red.
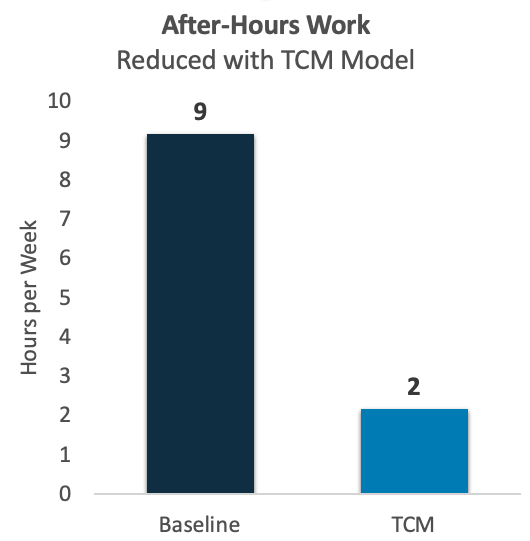
A better and more financially sustainable solution is to implement the Team Care Medicine (TCM) Model. The TCM Model is gaining traction nationwide and has been proven to significantly boost physician productivity and reduce/eliminate physician overtime (often referred to as “pajama time”). For example, a six-doctor primary care practice in the Midwest launched the TCM Model and within six months had reduced average “pajama time” by nearly 80% (see below).
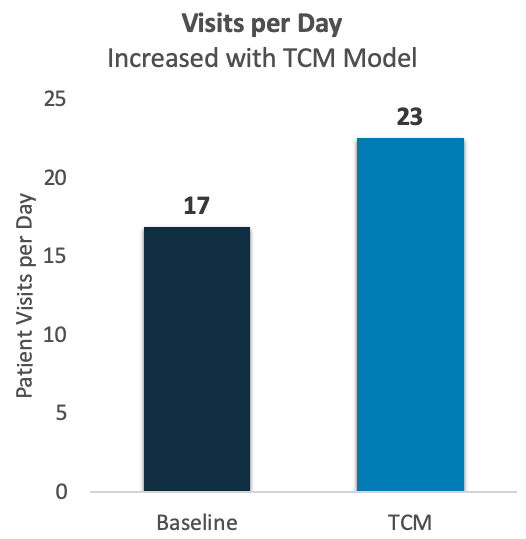
Even as they reduced after-hours work, these providers were able to see more patients each day. As illustrated below, their average visit volume increased by 35%.
Best of all, these physicians are experiencing a restored “Joy of Practicing Medicine”. They’re reestablishing connections with their patients and with their families. Remarking on happy physicians, happy patients, and happy administrators, one doctor called it a “Win, win, win!”
After launching the TCM Model, Dr. Miller abandoned his plan to switch to concierge medicine. With his charts current before the end of each workday, he’s started exercising again and is enjoying a long-term romantic relationship. This was unthinkable just 6 months earlier!
The TCM Model has been implemented in hundreds of doctor’s practices across the country. Here are just a few of their comments about its benefits.
“The executives and administrators see the upside of increased productivity, the quality of care is better and I’m having fun. I enjoy practicing medicine again.”
Patrick Anderson, MD
Richmond, IN
“[Now] I go home with nothing to do but play with my children and I have no reason to come in on Saturday.”
Travis Howell, MD
Winston-Salem, NC
“I realized this was the model we needed to adopt. Not only for our patients, but also for our own well-being.”
William Byars, MD
Greenville, SC
“As for my personal side, the TCM Model allows me to have a life outside of medicine, which I didn’t have before.”
Dick Albert, MD
Mebane, NC
“I love it…I am having ‘fun’ again!”
Jerry Dempsey, MD
Cincinnati, OH
In the TCM Model, the role of the physician is upgraded from overloaded work horse to team captain. The clinical support staff (usually MAs) are equipped to operate up to the limit of their license, performing 7 new skills that relieve the physician of unnecessary administrative burden. With a larger team of higher functioning clinical support staff, the physician is able to focus on the patient (not the EHR), to focus on diagnosis and care decisions (the reasons they went to med school), while the MA experiences more meaningful work and the practice enjoys higher revenues. For more information, go to www.wordpress-603318-1953014.cloudwaysapps.com.
By now, nearly all medical executives understand that their physicians are burning out at an alarming rate. However, very few grasp the full economic cost to their system. When a physician resigns, the replacement recruiting costs and the direct opportunity costs of missed patient visits are fairly obvious, but these account for just half of the overall financial impact to the system. Early retirement causes an expensive ripple effect which is often overlooked. And for the burned out physicians that have not yet quit, the malpractice risks to the system are substantial. In the context of primary care, these elements are explained and quantified below. We conclude that a burned out primary care physician creates an actuarial cost of increased malpractice risk of $37K per year and that the early retirement of a primary care physician triggers a loss in excess of $1.0MM to the system. The assumptions, sources, and calculations behind these conclusions can be found in this Excel spreadsheet.
Of course, this analysis still omits the human side of burnout, which will be discussed in a future article.
Burnout manifests in physical and emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. Sadly, this has become a nationwide phenomenon, affecting upwards of 44% of physicians.
The undisputed drivers of physician burnout are the EHR and related non-physician work. Physicians find themselves staring at the computer screen instead of engaging with their patients face to face. As documentation requirements for billing, for compliance, and for meaningful use standards continue to climb, their take-home work (e.g. “pajama time”) consumes their evenings. As a result, their personal lives suffer and work becomes all-consuming.
Sadly, when a physician begins to experience burnout, patient health is jeopardized. The 2019 Medscape Survey revealed 26% of depressed doctors say they are less careful when completing the visit documentation and 14% said they are making errors they wouldn’t ordinarily make.
At TCM, we have encountered burned out physicians running up to 6 weeks behind in closing their charts! For medical malpractice trial attorneys this circumstance is a “dream come true”, making the line of questioning about chart accuracy an easy path to large jury awards.
Survey results in a recent Mayo Clinic Proceedings article suggest a burned out doctor is 120% more likely to make a medical error than a doctor that is not. Not only does this jeopardize patient wellbeing, it also substantially elevates the risk of malpractice lawsuits. We calculate the actuarial risk at an incremental $37K per year per burned out doctor. Though most systems provide malpractice insurance for their physicians, these incremental claims translate into higher premiums and higher deductibles that hit the bottom line.
Burnout drives attrition, which is more expensive than you think
Replacing a physician is a costly and time-consuming endeavor. Recruiter fees typically run one-third of base salary, whether an external cost or an internal overhead charge. A typical signing bonus is 15% of base salary. When training and legal costs are included, we see $161K in direct hiring expenses.
The loss of a tenured primary care physician leads to significant direct revenue loss as the panel disperses and patients must see another provider for their care. The direct revenue loss can be split into two phases.
First, while the position remains open, there is an obvious loss of revenue. In most cases, TCM has seen other providers in the practice shouldering one-third of the visits that would otherwise have been taken by the lost physician (adding to their own burnout risk). The remaining two-thirds is simply lost revenue. With primary care docs increasingly scarce, we see a typical recruiting period of roughly 6 months from day of resignation to first day of work for the replacement. The direct loss of revenue during the replacement hiring period averages $161K, during which time overhead charges continue to accrue.
Second, even after the position is filled, the new physician typically cannot restore the full lost panel on Day One. Instead, they ramp up to full capacity over a 2-year period, operating with a 30% smaller panel in Year 1 and a 15% smaller panel in Year 2. The direct loss of revenue during the ramp up period for the new physician, compared to the lost physician practicing at full capacity, is $193K.
Thus, between the replacement hiring period and the replacement ramp up period, the direct revenues lost by the system add up to $354K.
When contemplating the cost of a lost physician and the merits of investing in physician wellbeing, corporate finance teams often overlook the lost referral revenues when a physician resigns. Here, too, the costs are borne during both the replacement hiring period and during the replacement ramp up period. ReferralMD reports that, after accounting for referral leakage, the average physician generates $672K per year in referral revenue to their system. During the replacement hiring period, this translates into $224K in missed revenues, even after accounting for some incremental visit volumes for the other physicians that retained one third of the panel. Likewise, during the replacement ramp up period, the system loses referral revenues of $302K. Combined, $526K of downstream referral revenues are lost by the specialists in the system when a primary care provider burns out and quits.
When a burned out physician finally quits, it costs the system $1,042K after all the costs enumerated above are tallied up. And prior to quitting, the physician costs the system an extra $37K year-in and year-out in elevated malpractice risk. Investing against burnout is not only the right thing to do, it’s the rational thing to do.
Against a panoply of half-measures and flawed approaches, one solution stands out as an empirically-proven solution to burnout. The TCM Model is gaining traction nationwide and has been proven to significantly reduce or completely eliminate physician overtime (often referred to as “pajama time”). Survey results from TCM clients consistently show significant gains in provider satisfaction as the provider is freed from the myriad administrative tasks that weigh them down and enabled to focus on the patient face-to-face again. Numerous physicians that have deployed the TCM Model have put off planned retirements to practice longer and have cancelled plans to move to a concierge practice, saving their systems millions.
The TCM Model was developed by Dr. Peter Anderson in Yorktown, Virginia. Prior to developing the TCM Model in his practice, he was one of the 383,250 doctors totally burned out, frustrated and hating medicine. Once perfected, the TCM Model allowed him to triple his revenues, become the highest revenue producing doctor in his hospital system, and increase daily visit volume from 18 patients per day to 35 patients per day. The best part, though, was completing his charts before leaving the office so he could go home with nothing to do but enjoy his family time and relax.
Our COVID-19 crisis is greatly impacting all Americans, particularly our healthcare workers. We want quick answers to our COVID-19 questions. Primary care providers (PCP’s) are using telehealth to improve access, but are challenged to meet the surging demand. This crisis will be a catalyst to future expansion of telehealth services.
While sheltering in place, I decided to write this article about the COVID-19 crisis and expansion of telehealth services. I expect this will be the first in a series of articles about how this crisis is impacting our health system and all Americans.
American COVID-19 cases are increasing more rapidly than other countries (Country by Country graph). We will soon have more cases than China, Italy, or Spain. Our COVID-19 cases are growing exponentially, with New York State reporting nearly 50% of total cases (Source – Worldometer). During the past week, total US cases have increased from 6,400 to 54,800 (as of March 24th). Cases are doubling every 3 days!
Due to delays in testing, I believe we have significantly underreported our COVID-19 cases. New York has increased their testing from 1,000/day to 16,000/day. As other states ramp up their testing, I expect we will see their numbers grow exponentially.
During this crisis, telehealth can help us provide more convenient and safe health services. Providers face great risks in contracting coronavirus, due to exposure to undiagnosed patients. Telehealth enables providers to minimize contact with COVID-19 patients. On the other hand, patients want to avoid a clinic waiting room full of potential COVID-19 patients. Telehealth provides patient visits at home on their smart phone.
I reviewed health systems offering telehealth services in the SF Bay Area, Seattle Puget Sound, Milwaukee, and Philadelphia (all places where I have lived). Kaiser now provides more telehealth visits (through email, phone, and video visits) than in-person visits. Although Kaiser has a well-established telehealth program, their video visits represent a small percentage of total telehealth visits.
Americans want to know, “How can I quickly get answers to my COVID-19 questions?” These health systems offer on-line symptom checkers and/or provide a phone number for initial screening and recommended next steps. Telehealth visits may be scheduled or provided on-demand. Because of increased demand, consumers can expect delays in arranging virtual visits with longer than normal wait times.
Health systems are ramping up telehealth services as quickly as possible. A major barrier to expanding telehealth has been the limited payments. In response to this crisis, the federal government has passed emergency regulations to improve telehealth payment and licensure requirements for Medicare services.
Our limited primary care provider (PCP) staffing will be a major challenge. We have a shortage of PCP’s with many working part-time to improve their work-life balance. Many PCP’s are over-whelmed by current practice demands and will have difficulty adopting new technology during this crisis. Health systems are freeing up PCP time by deferring elective visits and closing some of their clinics.
Well-established telehealth programs, such as Kaiser, Providence, and Penn Medicine, should have an easier time ramping up their services. They can offer the options of email, phone, or video visits. Their PCP’s are already very familiar with their telehealth systems. National telehealth companies want to quickly hire more PCP’s. But with our shortage of PCP’s, it may take months rather than weeks to hire additional PCP’s.
We must effectively utilize the time of our PCP’s, since they are at high risk for contracting COVID-19. We can more easily increase email and phone visits, rather than video visits. According to Dr. Ezekiel Emanual, we have fourteen days to defeat coronavirus and flatten the curve. After working through this crisis, we will determine how best to utilize telehealth and expanded care teams in providing more convenient, affordable health services.

Bruce Korus is the Founder of Korus Health Innovation. Expanded primary care teams will use telehealth to shift services from hospitals & clinics to homes & smart phones. Please send your comments to bruce@korushealthinno.com
All across the US, well-meaning administrators seeking solutions to physician burnout are turning to Team-Based Care (TBC) Models. Few understand that TBCs were not created for the purpose of combating physician burnout or restoring joy in medicine. Rather, they were developed in response to new payment models that incentivize gains in the overall health of the patient.
According to the Agency for Healthcare Research in Quality (AHRQ), “the primary goal of [Team-Based Care] is to optimize the timely and effective use of information, skills, and resources by teams of healthcare professionals for the purpose of enhancing the quality and safety of patient care”. While admirable and important, the primary intended beneficiary of TBC Models is the patient, not the physician.

The “team” in Team-Based Care refers to the primary care provider in addition to a host of adjacent healthcare professionals, such as care coordinators, triage nurses, pharmacists, and behavioral health professionals. For patients with complex health needs, coordination among these various providers is critical to good outcomes. However, when it comes to the mental well-being of the primary care provider, the TBC exacerbates the problem by adding more collaboration tasks and communication requirements to an already overwhelming workload.
A host of evidence points to excessive administrative burden and EHR data entry tasks as the primary drivers of physician burnout. Providers report that they spend much of each visit typing on the keyboard rather than looking the patient in the eye. Most cannot keep up with their charts during clinic hours, but instead try to catch up in the evening, depriving them of rest and a personal life.
Any cure for physician burnout must involve relieving the provider of a meaningful portion of this administrative burden, allowing them to focus on the patient and on the actual practice of medicine for which they were trained. Such assistance must come inside the exam room, where the history is collected, the exam is documented, and the charts are updated. With its focus on an outside the exam room team, TBC is barking up the wrong tree.
Many systems have turned to scribes as a mechanism to take the keyboard out of the hands of the providers, freeing them up in the exam room. While this approach clearly yields some benefits, it doesn’t fundamentally change the equation for the providers that still perform virtually the entire visit themselves. Schedule delays and long hours remain a problem, as the scribe is little more than a “human app” attached to the EHR, which still must be directed at all times by the provider.
In order to truly change the game for providers, they must be freed to focus exclusively on the parts of the patient exam that require someone with their level of training. Everything else must be delegated to qualified team members.
The Team Care Medicine (TCM) Model is built around this commonsense insight. In the TCM Model, the clinical assistants work ahead of and independent of the physicians. For instance, the clinical assistants gather all of the patient’s preliminary data, including chief complaint data, before the physician enters the exam room. They then present it to the physician verbally, in front of the patient, similar to how a resident presents a patient to their attending physician. The clinical assistants manage the EHR, including the capture of physical exam findings and recording of the diagnosis and treatment plan, thus freeing the physician to focus solely on the patient. The physician can then move on to the next patient, leaving the clinical assistant to provide patient education and close the visit.
The TCM Model enables the provider to spend less time on each patient, and thus see more patients per day. In order to keep the provider fully occupied at this higher level of efficiency, most practices hire one additional MA per provider. The cost of this additional team member is easily covered by the 20-40% increase in provider productivity, and by improved provider satisfaction and retention as they re-engage personally with their patients during the exam and no longer take charts home in the evening.
The principal drivers of physician burnout are found inside the exam room, so any solution must also transform the process and responsibilities inside the exam room. While there are admirable goals and benefits to a Team-Based Care Model, healthcare leaders seeking a solution to physician burnout would do well to consider the commonsense and empirically validated approach: the TCM Model.