Extra Staff Encourage Doctors to be More Mindful
Insistent job pressures cause two-thirds of physicians to experience burnout at some point during their career. As a result, more errors are made and a sense of empathy for patients is lost. In part, this is what’s causing physicians to leave clinical practice all together.
Mindfulness is one of the only known and proven remedies for physician burnout, but it’s not a cure all either. Mindfulness is the ability to be fully present and attentive in the moment; it’s an awareness.
According to a study, patients tended to be more open and satisfied when their physician was focused on their needs and not obviously distracted. Furthermore, mindful physicians were typically more upbeat and concentrated during patient interactions, while less mindful physicians frequently missed opportunities to be empathetic and failed to pay attention.
Danni Alcorn, a Health Writer for Emmi Solutions recently blogged about a personal doctor visit. To give you a little bit of background, Danni graduated from Northwestern where she double majored in pre-med. She considers herself health-literate.
On this particular morning, she writes about how she had been very sick for several days, sleep deprived and delirious. The physician entered the exam room where she was waiting and spouted off several questions to familiarize themselves. She learned that Danni was a recent pre-med graduate and that’s when the visit made a turn for the worse.
“As a patient, I needed to hear my treatment plan explained slowly in simple language. I needed a printout to take with me to remind me of her instructions hours or even days after I left her office. And I needed someone to check with me to make sure I’d actually understood the instructions I’d been given.” Danni writes.
Danni’s experience further proves that some physicians are determined to stay on their focused path of seeing patients, documenting what medical data needs to be documented and moving onto the next patient day in and day out.
Did you know that 80% of what patients hear, they forget by the time they reach the parking lot?
The issue is not whether physicians want to be mindful, it’s that they are distracted by the many patients they have previously seen, wondering if the recommendations they made were best, remembering they have forgotten to call in an order or call back a patient. Their minds are always working and it prevents them from being mentally present.
Back in 2002, when I was practicing medicine at Hilton Family Practice in Newport News, VA, I found myself experiencing similar situations. It was all I could do to get through the day, then to realize that it all had to be repeated when I woke up the next morning was depressing.
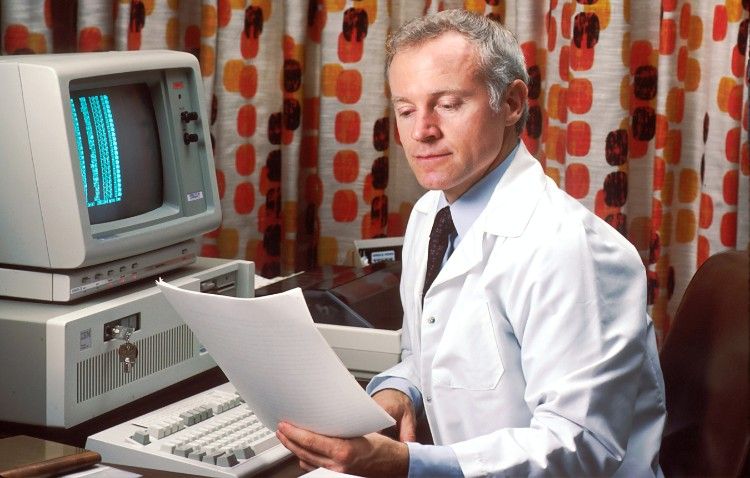
About a year later, with the help of two of my nurses, I decided to change the workflow of my office, primarily the patient visit. I elevated the responsibilities of my nurses to include gathering data, scribing patient visits on the EMR, and educating patients. This ultimately relieved me of responsibilities that did not necessarily require my expertise as a physician and allowed me to devote my full attention on each and every one of my patients.
I quickly experienced a more efficient exam room dynamic, increased quality of care, documentation was complete and competent and financial performance sky rocketed. Moreover, I started enjoying practicing medicine again and my staff was experiencing the same professional satisfaction.
Having extra staff to help with documentation enables physicians to be more mindful because its takes many of the tedious responsibilities off of their back and out of their mind.
Dr. Mary Catherine Beach, lead author of the study and an associate professor of medicine at Johns Hopkins University said, mindfulness “…allows doctors to help patients by listening more, talking less, and seeing what the patient needs.”
Adopting a sense of awareness while interacting with patients benefits both the doctor and the patient and is essential in nurturing this doctor-patient relationship. The Family Team Care model offers a way to improve physician’s ability to be “mindful” of their patients and reduce burnout.